Macular Edema Symptoms & Diagnosis
Your Local Ophthalmologist Specialized in Retina
Neighborhood Retina Care Doctors in Sarasota, FL
Retina Specialists Providing Treatment for:
Macular Edema Symptoms and Diagnosis
Macular degeneration is not the only retinal condition that threatens central vision with age. In fact, there are many reasons for swelling to show up in the macula, and it takes an ophthalmologist specialized in retina to determine the cause and recommend the correct treatment. Shane Retina is specialized in diagnosing and treating the many causes for macular edema in Sarasota and Manatee Counties.
What Is the Macula?
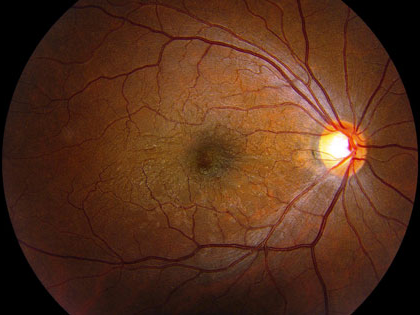
The retina is a thin structure that lines the inside back surface of your eyeball. The entire surface of the retina is around two square inches. The central 5% of the retina, where vision is sharpest, is called the macula. Light enters the eye through the pupil and is focused by the lens onto the macula to create reading and driving vision.
What Is Macular Edema?
Macular edema is another word for macular swelling. Macular edema comes from leaky blood vessels that course below, above, or within the retinal layers. On a microscopic level, abnormal retinal blood vessel walls allow fluid to pass from the bloodstream into the retina, distorting the normal retinal architecture.
There are many causes for macular edema. In most cases, the retina is injured, inflamed, infected, or experiencing low blood flow. These mechanisms lead to the release of chemical signals that modify the integrity of the blood vessel walls. Interestingly, while the blood vessels allow fluid to escape, the gaps in the vessel walls are not typically large enough to allow for bleeding.
What Retinal Conditions Lead to Macular Edema?
The most common conditions that lead to macular edema are macular degeneration, diabetic retinopathy, and retinal vein occlusion. There are other common, but less well-known causes for macular edema, including hypertension, cataract surgery inflammation and uveitis. With these three conditions, the swelling that occurs is called cystoid macular edema (CME).
When a patient experiences extended periods of extremely high blood pressure, the retinal vessels can leak fluid. This would be analogous to the leakage that would occur if an old garden hose were put under too much water pressure. Sometimes the blood vessel wall protrudes, called a macroaneurysm.
CME is one of the most frequent side effects of eye surgery, particularly cataract surgery. Ophthalmologists currently believe that this retinal leakage occurs due to post-surgical inflammation that causes macular vessels to leak. It typically appears a few weeks following cataract extraction, notable to the patient as an unexplained worsening of central vision. Up to 50% of patients experience cystoid macular edema after cataract surgery, but only a handful require extended treatment by a retina specialist. In most cases, CME resolves over time with or without treatment.
Another cause for cystoid macular edema is uveitis, a generic term for inflammation in the eye. There are many countless reasons for an eye to be inflamed, but most fall under the category of infections or autoimmune conditions, where the body’s immune system attacks its own tissue. Uveitis is a complex process requiring lab work-up and other specialized testing to determine the proper diagnosis and treatment.
Rarely, cystoid macular edema can occur without infection or inflammation. This so called ‘non-leaking’ CME may be due to inherited retinal disorders, epiretinal membranes, or too much vitamin (niacin) supplementation.
What Are the Symptoms of Macular Edema?
Macular edema causes painless blurring of central vision in one or both eyes. In some cases, the eye may be red or sensitive to light. The symptoms may fluctuate over time. Macular edema does not cause transient loss of vision, double vision, or eye irritation. The condition may be associated with a history of autoimmune disease or recent eye surgery.
How Is Macular Edema Diagnosed?
If the ophthalmologist is unsure of the source of the macular edema, he may order additional images with a camera technology called fluorescein angiography. This test involves injecting dye into an arm vein and taking pictures at it flows through the retinal vessels. Any swelling withing the macula glows brighter as the test progresses, sometimes revealing the source of the leakage.
Anyone who suspects that they may have macular edema should seek a dilated exam with an ophthalmologist, preferably one specialized in macular and retinal conditions. During your appointment, your vision will be checked, and eyes dilated. Specialized images of your retina using optical coherence tomography (OCT) will be obtained. Then the ophthalmologist will examine your eyes with a lighted microscope before discussing diagnostic and treatment options with you.
If there is inflammation in the eye, the eye doctor may order lab testing to look for common infections or autoimmune conditions that manifest in the eye.
How Is Macular Edema Treated?
Correctly diagnosing the underlying cause for macular edema is critical to instituting the appropriate treatment. For macular degeneration, injections of medication are first choice. Hypertension, diabetic retinopathy, and retinal vein occlusion also benefit from injections, but in conjunction with blood sugar and blood pressure control.
When cystoid macular edema occurs after cataract surgery, the first-line therapy involves drops of steroid and ibuprofen-like medication. If these treatments are found to be insufficient, steroids can be injected directly into the eye. Typically, the need for these therapies goes down over time.
When uveitis (eye inflammation) is the main cause for retinal swelling, steroid drops are commonly the initial treatment until lab results come back. Depending on the infection or autoimmune condition that is identified, a patient may be treated with antibiotics, antivirals, steroid injections, oral steroids, or even steroid-sparing immune suppressants. Sometimes, a rheumatologist is consulted for management of any systemic medications.
What Are the Side Effects of Treatment for Macular Edema?
The goal of treatment for macular edema is to restore vision without otherwise harming the eye. The various treatments mentioned previously are all considered safe, but the ophthalmologist will be on the lookout for well-known side effects.
Some prescription drops can become irritating to the eye or cause a surface allergy. When steroid medication is used to treat macular swelling, eye pressure can become temporarily elevated. These patients may have to be treated with pressure-lowering drops and watched for the onset of glaucoma. For eye injections, there is a 1/5000 risk for infection, which can be blinding.
When systemic immune suppressants or steroids are used, a whole host of familiar side effects are possible. Anyone who takes oral or injectable medications for macular edema should be followed in consultation with their primary care doctor or rheumatologist.
What Are the Outcomes After Treatment of Macular Edema?
Most patients successfully rid themselves of retinal swelling with the appropriate treatment and time. Even those who are not able to eliminate their macular edema are able to stabilize their vision with ongoing treatment.
Your Macular Edema Specialists in Sarasota And Manatee
Shane Retina, is specialized in managing macular edema. If you experience the symptoms mentioned above, consider having a dilated eye examination with an ophthalmologist. This exam may involve photographs or other specialized imaging tests of the retina. There are effective treatments for macular edema, so do not delay your evaluation.
For more information regarding age-related macular degeneration, please visit the American Society of Retina Specialists patient information website: http://www.asrs.org/patients/retinal-diseases/20/macular-edema or click on links to articles written by our retina specialists below.
