Diabetic Retinopathy Symptoms & Diagnosis
Neighborhood Retina Care Doctors in Sarasota, FL
Retina Specialists Providing Treatment for:
Diabetic Retinopathy and Eye Disease
One in ten Americans has diabetes. This condition is characterized by elevated blood sugar levels, which damages blood vessels and reduces blood flow throughout the body. One of the most devastating consequences of diabetes is the way it can rob people of their vision. In fact, diabetes is the leading cause of vision loss between the ages of 20 and 64. Fortunately, there are treatments available today that can reverse vision loss from diabetes. The trick to preventing blindness is to get people educated, evaluated, and treated before it’s too late.
How Does Diabetes Affect the Eye?
 Underlying all bodily harm from diabetes is the fact that elevated blood sugar causes blood vessel damage. Fine blood vessels in critical organs such as the eyeball are particularly vulnerable. Over time, these vessels become leaky, bleed, and unable to transmit blood and oxygen to the tissues they serve.
Underlying all bodily harm from diabetes is the fact that elevated blood sugar causes blood vessel damage. Fine blood vessels in critical organs such as the eyeball are particularly vulnerable. Over time, these vessels become leaky, bleed, and unable to transmit blood and oxygen to the tissues they serve.
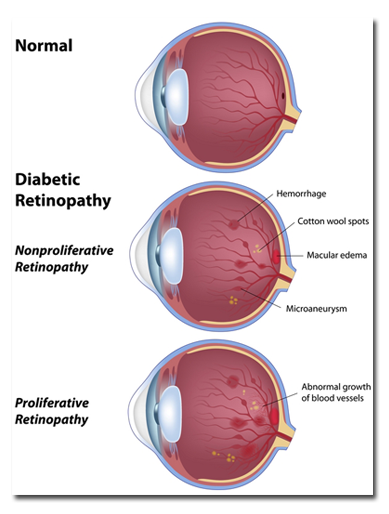
In the retina, tiny vessels are critical to supporting the robust metabolism that is required to create vision. As the walls of these vessels become less water-tight (think of an old, leaky hose), fluid can escape and accumulate within in the layers of the retina. This leads to swelling and distortion of the retinal layers in the center of the vision, a condition called diabetic macular edema (DME). Diabetic macular edema is the leading cause of vision loss in diabetics.
As years of poor blood sugar control take their toll, the retinal blood vessels lose the ability to provide adequate oxygen to the eye. In this ‘oxygen-starved’ state, the eye begins releasing chemical signals to stimulate new blood vessel growth. The most important of these signals is called vascular endothelial growth factor (VEGF).
In response to elevated VEGF, the retina begins to grow new blood vessels, also known as neovascularization. The presence of neovascularization marks the most advanced stage of diabetic eye disease, called proliferative diabetic retinopathy. Unfortunately, these new vessels grow in an uncoordinated fashion, pulling and disrupting the retina’s delicate structure. The vessels also bleed spontaneously, causing rapid onset of dark floaters and loss of vision. Eventually, the new blood vessels pull and detach the retina, leading to severe and permanent vision loss.
What Are the Symptoms of Diabetes in the Eye?
The most common initial symptom of diabetic retinopathy is painless blurry vision in one or both eyes. Be careful to test one eye at a time because sometimes the stronger eye will cover for the weaker one. Occasionally, a diabetic may experience the sudden onset of floaters, which represents bleeding in the jelly that fills the eye. Rarely, elevated pressure and pain may occur in advanced cases.
Diabetic changes in the eye can be asymptomatic for a long time. Asymptomatic does not mean all is well, however. Too many patients wait until after they get symptoms to see an eye doctor. By that time, some of their vision may be permanently lost regardless of treatment.
I have diabetes. Should I see an ophthalmologist?
The American Academy of Ophthalmology recommends that adult diabetics should receive a dilated examination by an eye doctor every year. These examinations will be looking for signs of blood vessel damage, growth of new blood vessels, or swelling of the retina that threatens vision. Many of these changes can be asymptomatic initially but lead to bigger problems if they are not identified early.
What Happens During My Eye Examination?
On the day of your eye examination, you will be greeted by our staff at the front desk and given a one-page medical history form to complete. Afterward, a technician will escort you to a private room where your vision is checked, eye pressure measured, and pupils dilated. The next step is to obtain an image of the retina called an OCT, which allows the doctor to see microscopic details of your central retina.
The doctor will examine your eyes with specialized lights and equipment, review your pictures, and share his assessment with you. This is a good time to ask any questions you may have about diabetes and your eye health. If treatment is required, the doctor will discuss the risks, benefits, and alternatives before proceeding with our vision-saving therapies. The entire visit is usually complete within 1 hour.
What Sorts of Treatments are There for Diabetic Retinopathy?
Ophthalmologists now have a multitude of treatments to prevent vision loss from diabetes. Each treatment has unique benefits and risks that must be considered when deciding how to proceed with therapy. But rest assured, with regular follow-up and treatment, you stand a good chance of keeping the vision you need to drive, read, and work.
The most powerful treatment for diabetic retinopathy is the most obvious: good blood sugar control. The better you control you blood sugar, the less risk you will have for vision loss. Controlling other cardiovascular risk factors helps as well, including blood pressure, cholesterol, smoking, exercise, and weight.
Once diabetic retinopathy progresses to retinal swelling (diabetic macular edema) or new blood vessel growth (proliferative diabetic retinopathy), further treatments become necessary. One treatment option is retinal laser, which is a 10 minute procedure performed in the clinic. Retinal lasers have the advantage of long-lasting reduction in vision loss from diabetes. However, they have the disadvantage of intentionally damaging the peripheral retina in an attempt to protect central vision.
Laser for Diabetes
In advanced cases of diabetic retinopathy, it may become necessary to perform surgery on the retina. Sometimes, the eye is full of blood, which must be removed using a procedure called ‘vitrectomy,’ or removal of the vitreous jelly that fills the eye. It is common during these procedures for laser to be applied to the peripheral retina to prevent further bleeding after the surgery. Sometimes, diabetic retinal detachments are repaired using additional maneuvers inside the eye.
Eye Injections
Another treatment option for diabetic retinopathy is injection of medication in the eye. The most common medication used in diabetes is called anti-VEGF, which goes by the brand names Avastin, Lucentis, or Eylea. These medications suppress retinal swelling and blood vessel growth without causing permanent damage to any eye structures. The downside of eye injections is that they have to be repeated to maintain their effect, sometimes as often as every month or two. In some cases, steroids are injected into the eye, which also suppress retinal swelling, are longer lasting, but may cause cataracts or glaucoma as a side effect.
Diabetes is a difficult disease that has many life-changing side effects, including vision loss and diabetic eye disease. Diabetic retinopathy treatment, a service provided by Shane Retina to patients in Sarasota and Manatee county, can improve and prevent vision loss due to diabetic eye disease.
Care for Diabetic Vision Loss in Sarasota & Manatee County
Shane Retina specializes in diabetic retinopathy treatments and diabetic retinopathy surgery in Sarasota and Manatee County. If you have diabetes, consider having a dilated eye examination with an ophthalmologist. This exam may involve photographs or other specialized imaging tests of the retina. There are effective treatments for most forms of diabetic retinopathy, so don’t delay your appointment until you are experiencing changes in your vision.
Read more about the New Treatments for Vision Loss in Diabetes here.
For more information regarding diabetic retinopathy treatments, including diabetic retinopathy surgery in Sarasota and Manatee County, please contact us and visit the American Academy of Ophthalmology patient information website: http://www.asrs.org/patients/retinal-diseases/3/diabetic-retinopathy.
