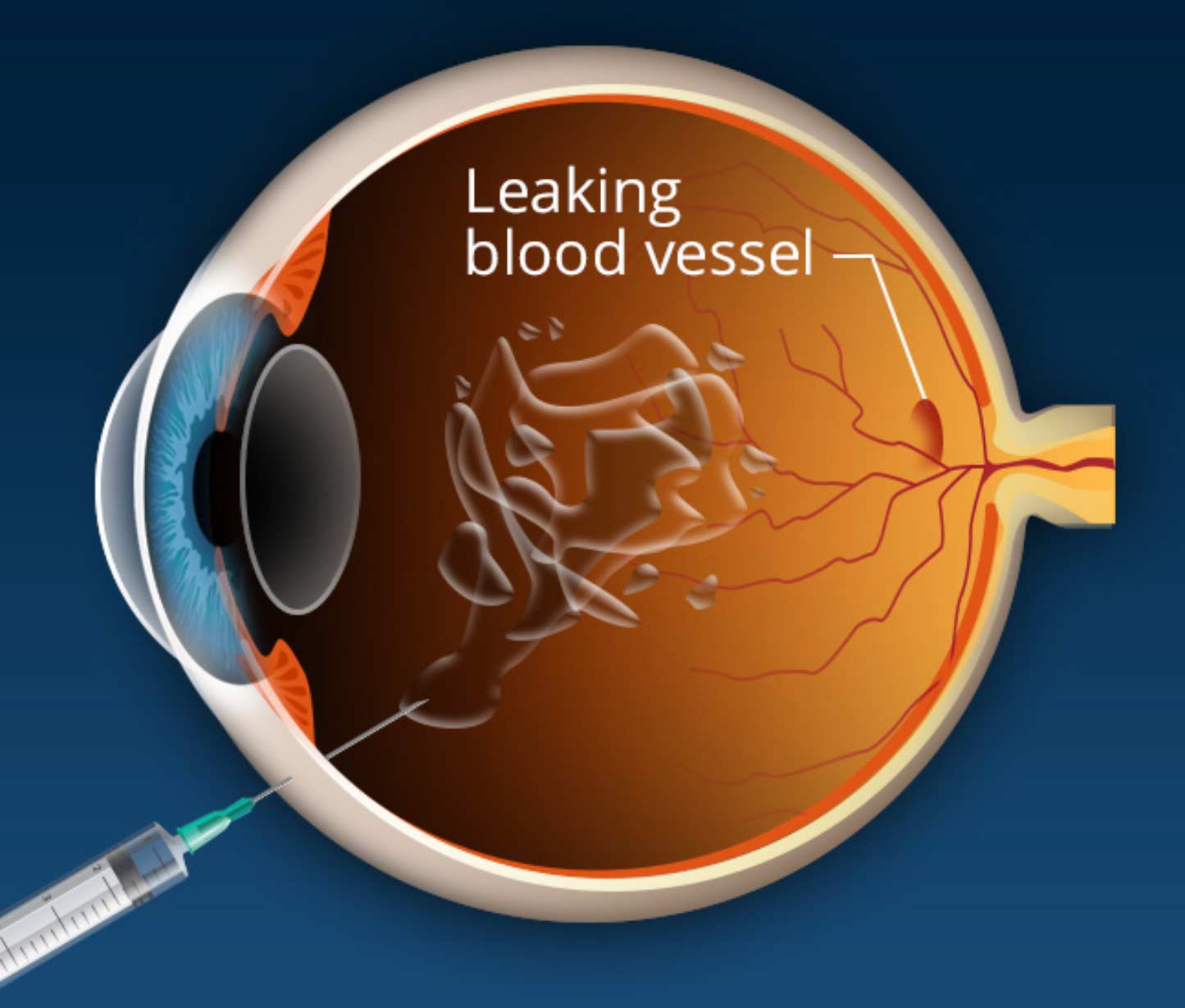
Over the last decade, intravitreal injections have become the mainstay of treatment for numerous retinal conditions. An intravitreal injection is an in-office procedure in which medication is placed directly into the vitreous – the gel-like fluid that fills the eye. This procedure treats severe retinal conditions by administering a high level of medication directly to the retina.
What are Intravitreal Injections Used For?
Intravitreal injections are used to treat a variety of retinal conditions associated with severe vision loss. These conditions include age-related macular degeneration, diabetic retinopathy, and retina vein occlusions. Additionally, intravitreal steroids are used in some patients experiencing swelling in the retina caused by cystoid macular edema, diabetic macular edema, uveitis, or other inflammatory conditions. Antibiotic, antiviral and antifungal medications can also be injected into the eye to treat patients with eye infections such as retinitis and endophthalmitis.
Source: https://www.asrs.org/patients/retinal-diseases/33/intravitreal-injections
Types of Injections
There are three common drug types that can be injected into the eye to treat specific retinal conditions. These drugs include:
Anti-VEGF drugs
Vascular endothelial growth factor (VEGF) is a protein that tells the body to grow new blood vessels. The process of growing new blood vessels is known as neovascularization. Individuals with retinal conditions such as age-related macular degeneration or diabetic retinopathy grow these abnormal weak blood vessels causing disruption in their vision.
Anti-VEGF medications when injected into the eye, inhibit the growth of these blood vessels ultimately improving or preserving vision. To keep these blood vessels at bay, continued injections may be required.
At the start of treatment, it is common to receive injections of anti-VEGF medications once a month. However, over time you may need injections less often. Many individuals are able to discontinue injections altogether. The most common anti-VEGF medications include Eylea, Avastin, Lucentis, and Vabysmo.
Steroids
Patients experiencing active inflammation that is uncontrolled by topical therapy may benefit from an intravitreal steroid injection. Conditions of inflammation in eye include cystoid macular edema, scleritis and uveitis. Your retina specialist may suggest this injection to allow a high level of medication to the retina. Common steroid medications include Ozurdex, Triescence and Kenalog.
Antibiotics, antiviral and antifungal
Entry of any infectious material into the eye can have detrimental effects to your vision. The best way to treat these types of infections is through an intravitreal injection of antibiotic medication. This method allows the best access to the site of infection. Common conditions treated include endophthalmitis and retinitis. Medications that can be administered for eye infections include ceftazidime and vancomycin.
How are Injections Performed?
You may be asking yourself, “how does the medication get into my eye?” First and foremost, it is important to note that this procedure is an in-office procedure performed by a retina specialist. Once your retina specialist has determined that you have a condition that would be better treated by an intravitreal injection, they will walk you through these steps.
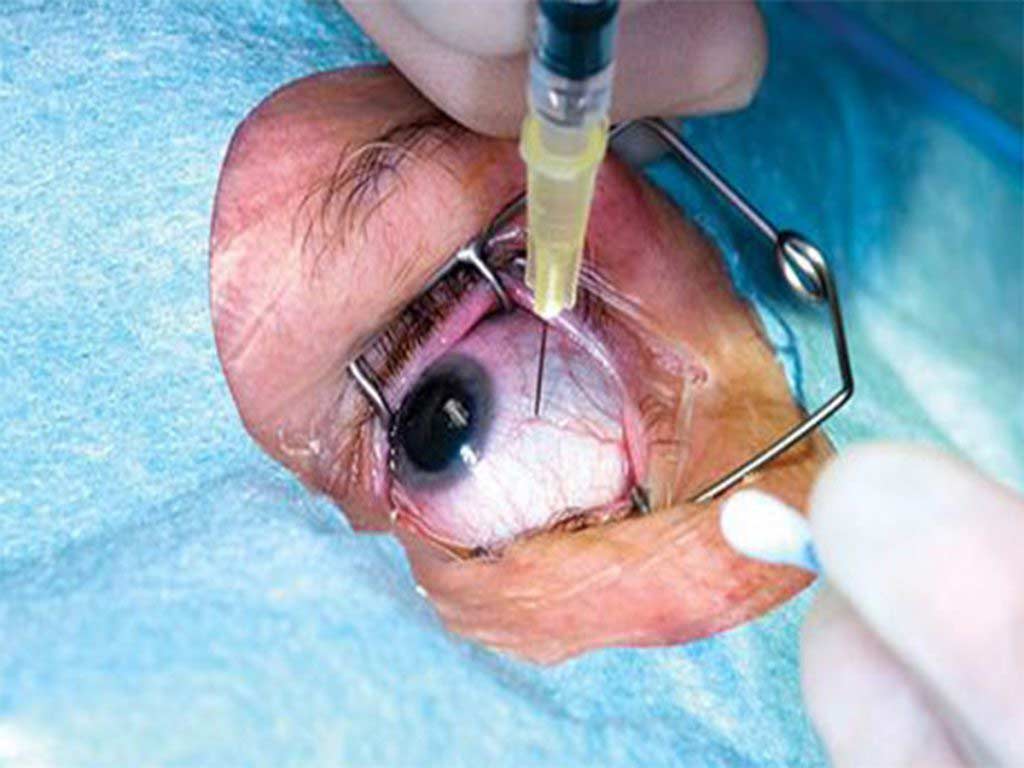
The patient will be reclined back in an exam chair and a numbing drop or gel will be placed on the white part of the eye. This ensure that the patient feels minimal pain during the injection. Next, a drop of betadine will be place at the injection site. This step is crucial as it the first step in preventing bacteria that lives on the surface of the eye from entering the injection site. Some retina specialist will use a betadine swab on the lash line for extra protection against bacteria. An eye lid speculum is then placed in the eye to keep the eye open during this short procedure.
Once prepped, you will be asked to look in a specific direction so the medication can be administered with a small needle. The site of the injection is located in the pars plana, the white part the eye.
At the time of the injection, you may feel a small pinch and pressure while the medication goes into the eye. Once completed, the speculum is removed and the eye is cleaned of all antiseptic material. The entire process can take anywhere from 10-15 minutes.
What to Expect after an Injection:
There are little to no restrictions following and intravitreal eye injection. Patients should avoid exposing the eye to potential contaminants the day of the injection. Experiencing side effects after an injection are minimal. However, some patients may experience small floaters or a bubble in the eye. This is cause by microscopic bubbles within the medication itself.
Additionally, patients may also feel some discomfort on the surface of eye caused by the betadine drops. Typically, a round of artificial tears over the next 24 hours will reduce any irritation.
What are the Risk Factors?
Understanding all the risk factors associated with any procedure is crucial. As with any procedure, intravitreal injections do have their risk. Although severe complication is uncommon, the most important risks include:
- Infections in the eye (endophthalmitis)
- Vitreous hemorrhage – bleeding in the gel-like fluid in the back of the eye
- Inflammation in the eye (uveitis)
- Retinal detachments
Of the major risks, infection in the eye (endophthalmitis) is the most serious and must be treated immediately. If you notice worsening of vision or severe pain 1-7 day after an injection you should contact your retina specialist immediately. Treatment for this type of infection is and injection of a broad-spectrum of antibiotics and often times surgery to prevent further damage. Thankfully, due to the numerous measures to prevent infections during this procedure, an infection from an eye injection is less than one in 5,000.
Additionally, after an injection you may notice a small bleed on the surface of the eye known as a subconjunctival hemorrhage. This usually appears at the site of the injection and heals within a week. A temporary rise in the pressure of the eye may occur after an injection. Your retina specialist may elect to check the intraocular pressure over a period of time to ensure the pressure returns to its normal baseline. This usually occurs within a few minutes.
How many Injections will I need?
Determining the number of injections, a patient may need is difficult due to a variety of external factors. The specific retinal condition that is being treated plays a large role in the number of injections a patient may receive.
Once a condition has be identified, your retina specialist will discuss with you which form of medication is your best option. In some conditions such as age-related macular degeneration or diabetic retinopathy, patients can expect to receive a series of injections. In the beginning injections are typically spaced 4-6 weeks apart for these specific conditions. As the eye begins to receive medication, it may be determined that you can extend your injection interval a few weeks at a time.
It is important to note that each time a patient returns to the clinic for an eye injection, your retina specialist will take a specialized photo of the retina with an OCT machine. This photo provides a glimpse of how the retina is reacting to the medications you are receiving. Your retina specialist will use these photos each time to customize your treatment plan.
Ongoing research is underway to provide longer-acting treatments to reduce the number of injections a patient may receive.
Shane Retina is one of Florida’s leading retina specialist clinics. We have clinical personnel solely dedicated to giving you a comfortable, safe, and effective eye injection experience. Call us today to schedule an evaluation for macular degeneration, diabetic retinopathy, or retinal vein occlusion.

 Are you experiencing vision issues and not sure what is happening? At Shane Retina, we are retina specialists equipped to deal with the full range or retina issues. Contact us today to get help now!
Are you experiencing vision issues and not sure what is happening? At Shane Retina, we are retina specialists equipped to deal with the full range or retina issues. Contact us today to get help now!