Articles by Shane Retina
How Age Affects Our Vision — According to an Ophthalmologist
As retina specialists in the Sarasota and Manatee County area, we come into ...
How Ophthalmology Can Aid Diabetes
Diabetes and Eye Health: How Ophthalmologists Can Improve Your Quality of Life Despite ...
Family History of Eye Disease? This is Why Ophthalmologist Visits Are a Must
You might be surprised to hear that more than 350 retinal and eye ...
“The eye is the jewel of the body”
How to prepare for an ophthalmologist appointment
Did you know that nearly 1.3 million Americans age 40 and older are ...
Tips On How To Recover From Eye Surgery
Our eyes are one of the most sensitive organs in our bodies, but ...
Intravitreal Injections 101: What You Need To Know
Over the last decade, intravitreal injections have become the mainstay of treatment ...
What is a retinal tear (and is it as scary as it sounds)?
Even though we make it a priority to put our patients at ease, ...
7 Reasons to See an Ophthalmologist
In terms of our overall health, our eyes can play a crucial role ...
5 Factors To Consider When Choosing an Eye Clinic
Choosing the right eye clinic is a vital decision towards maintaining the health ...
What Makes A Good Ophthalmologist?
Many people get confused between ophthalmologists and opticians - they both help you ...
What You Should Know About a Cystoid Macular Edema
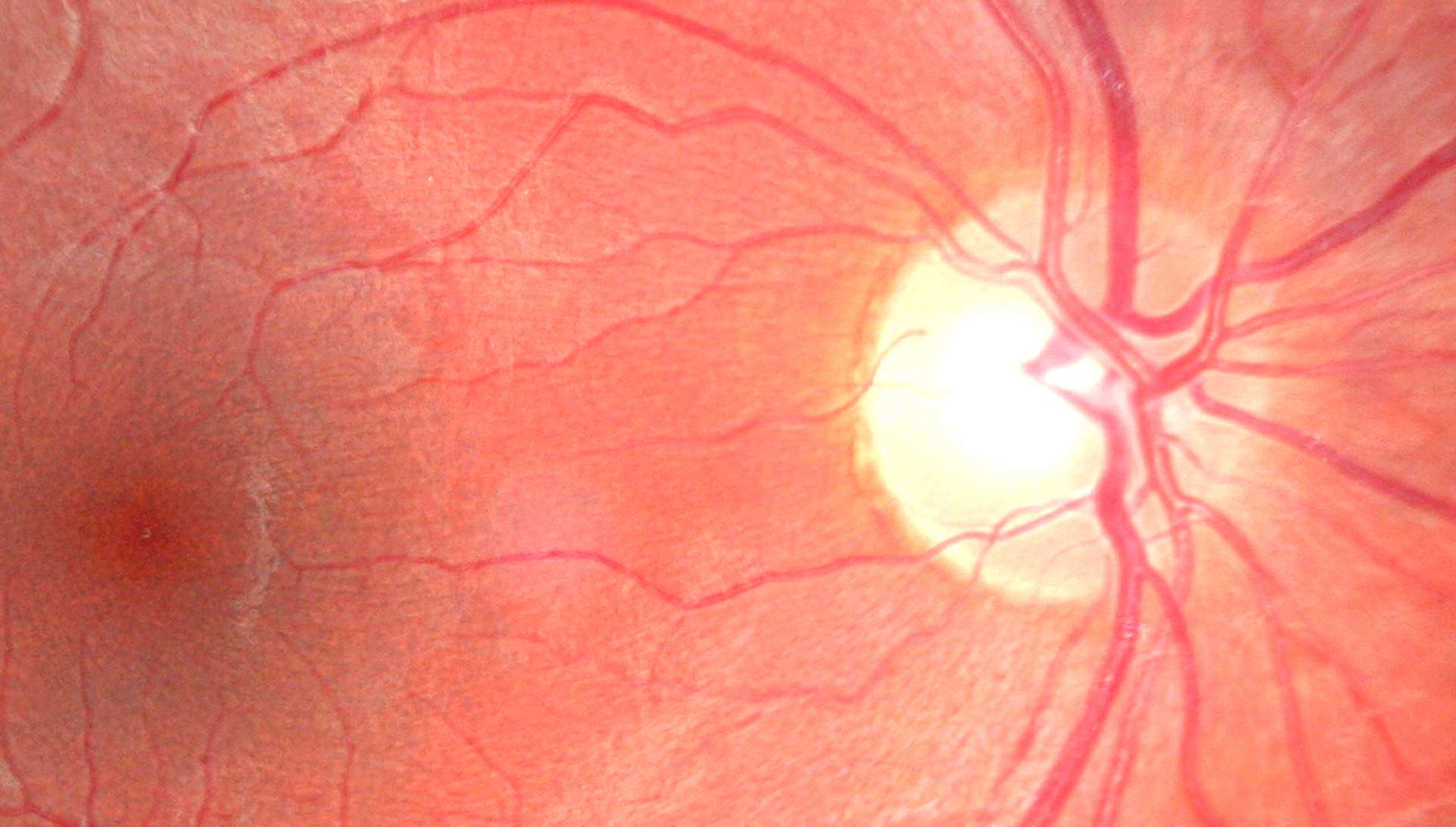
The thin light-sensitive tissue lining the back of the eye is known as ...
Understanding the Stages of Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes that affects the eyes. This condition ...